The Need
The current model of care for vulnerable populations is siloed across and within medical and social providers. Individuals who seek care from multiple agencies likely have a case manager to represent them at each provider, but these case managers lack the technology to collaboratively coordinate care across systems. As such, referrals between systems are passive, placing the responsibility of coordinating visits upon the most at-risk individuals.
50% of healthcare spending in the U.S. is consumed by just 5% of the population?
In order to get better, this 5% of high-cost patients often need social and behavioral supports that fall outside of the traditional medical domain.
To solve these issues, we have developed the Unified Care Continuum Platform, which bolsters population health at many levels to ensure accountability and coordination across provider systems.
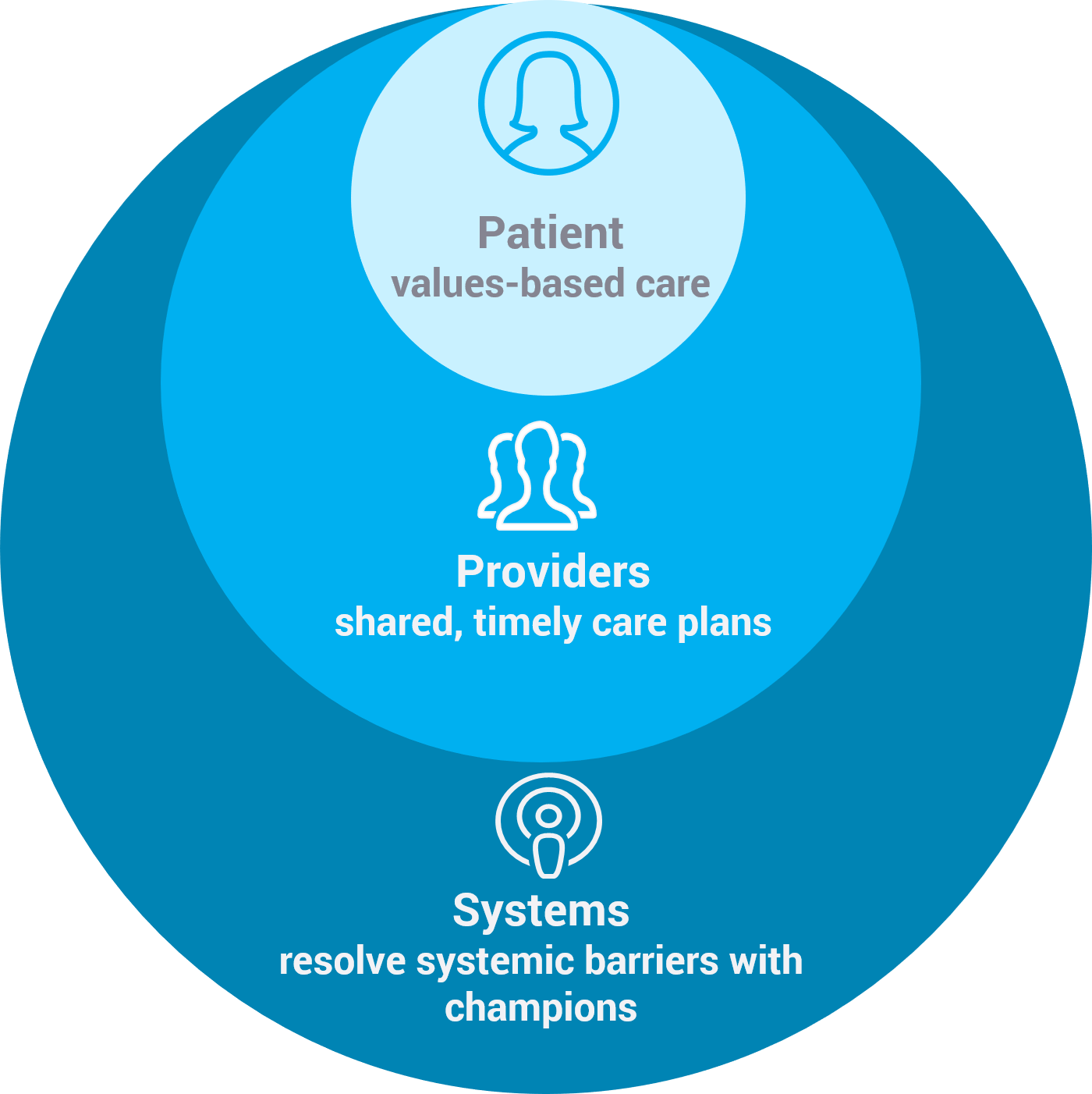
By following the evidence that 80% of an individual’s health is determined by social, economic and environmental factors, while 20% of an individual’s health is determined by clinical factors, our platform is designed to track, measure, and address these complex determinants of health – including medical, housing and transportation, income and employment status, hunger and access to nutritious foods, literacy and language, behavioral health, social integration, and much more – by linking data from disparate medical and social provider systems to create a comprehensive record for each client. We turn the current problem-centered model of care on its head by facilitating personalized care plans that are driven by clients’ values, goals, and strengths.
The Unified Care Continuum Platform’s core functionalities include facilitating care coordination for patients with complex needs, linking need to resources in real-time, streamlining collaboration between medical and social service providers, and generating data to support advocacy for systems-level change.
Platform Overview
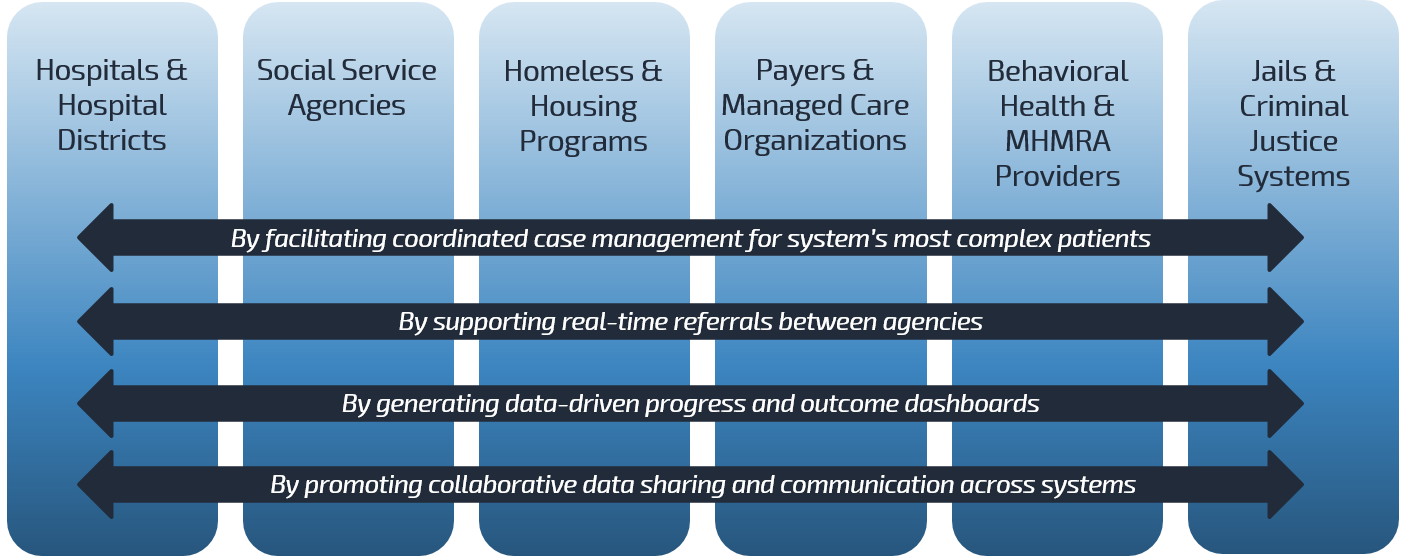
We are building a bridge between service providers to facilitate data sharing and cross-agency care coordination for Houston’s most vulnerable individuals. Through robust, cross-agency data analytics and patient care plans that are shared across agencies, our platform strengthens our region’s health safety net by empowering medical and social agencies to collaboratively address social and economic determinants of health.
Our platform leverages big data to drive targeted, patient-centered care coordination to improve health, social stability, and quality of life for Harris County’s most socially and medically complex patients. Read on to learn how our platform benefits medical and social agencies, patients, and policymakers.
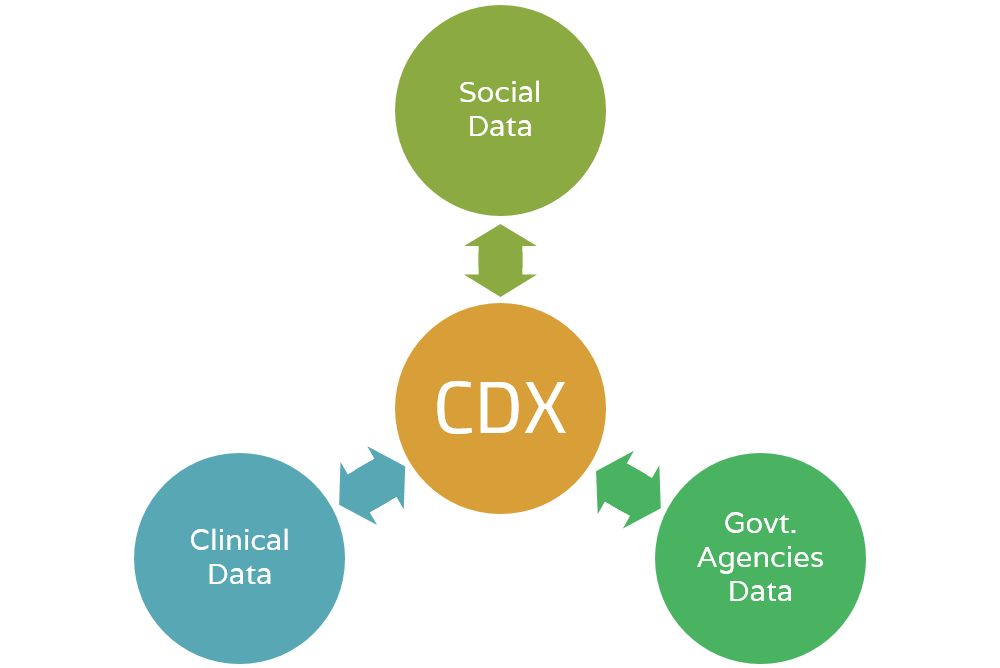
Community Data eXchange - Merges social and medical records
The Community Data eXchange is a data platform that merges patient data from medical and social service agencies. By linking data from over 8 million client visits to various systems (i.e. hospitals, EMS calls, homeless shelters, insurance companies, recovery/rehabilitation centers, and more), the Community Data eXchange bridges the communication gap between siloed systems and helps us see a more complete view of utilization and needs.
By using service utilization as an indicator of patient complexity, the Community Data eXchange helps healthcare providers and payers, social service agencies, and local governments understand population health needs and service gaps within a community. One way we use the Community Data eXchange is to identify the small number of individuals in a given population who rely on the greatest number of services. Using this measure a proxy for social and medical vulnerability, the Community Data eXchange informs the selection process for patients who stand to benefit the most from personalized care coordination, driven by patients’ values and goals.
-
The Community Data eXchange enables medical and social agencies to collaboratively recognize clients they have in common, identify common service gaps in the community, and work together to overcome systemic barriers to health. Because we understand health to be the complex interplay between social, behavioral, and medical factors, we must expand our definition of healthcare to include an integrated response across social, behavioral and medical domains. By linking patient records across social and medical agencies, the Community Data eXchange allows providers to see the specific social vulnerabilities of their patients alongside their pathologies. Since many medical conditions are exacerbated and even caused by social vulnerabilities, providers that understand their patients' complex needs are better equipped to engage with patients and develop effective care plans. The Unified Care Continuum Platform has built-in resource referral systems that enable providers from different agencies to collaboratively address social, behavioral and medical needs.
-
Agencies that provide social services to vulnerable individuals can partner with PCIC to discover how their client population utilizes other community services. This helps team deliver meaningful patient segmentation that considers social and medical risk factors for health. Our data discovery has helped social agencies understand how participation in their programs reduces the frequency and cost of participants’ emergency services, homeless shelter check-ins, jail bookings, and more.
-
On an individual level, the most socially and medically complex patients will be met with personalized care coordination to holistically address their health needs.
-
Our long-range strategy includes understanding widespread data on social and medical service utilization, a proxy for unmet need and disparity, as a means of informing policymakers of our community’s most pressing and unmet needs. Once the system can recognize, measure, and respond to the factors that affect population health, policies and procedures can be enacted to help overcome these systemic barriers to health.
Community Resource eXchange - Connects the right resource to the right person
The Community Resource eXchange exists to facilitate effective resource referrals between siloed medical and social agencies.
Developed in a collaborative API-based model, the Community Resource eXchange links existing resource databases (such as 211 or Aunt Bertha) with computerized inventories of local medical and social service agencies. It is a standardized, web-based platform that is interoperable with medical and case management software.
Examples of resources include appointments at clinics, open beds at various shelters, food and clothing inventory of local relief organizations, spaces available in recovery/rehabilitation centers, and more.
-
The Community Resource eXchange will have a live referral function, which serves as a warm hand-off between providers at different agencies. Providers will know that when they connect clients to resources, the resources will be there.
Connecting patients to appropriate community resources helps them overcome social and economic determinants of health (i.e. stable housing, access to nutritious food, reliable behavioral health services, etc.). Supporting patients outside of the traditional medical domain helps solve the root cause of health issues, and ultimately leads to fewer costly and avoidable Emergency Room visits and Hospital admissions.
-
On their own, social service agencies have limited resources (staff, shelter beds, case managers, meals, etc.), and as a result case managers often refer clients out to other agencies to fill service gaps. The Community Resource eXchange is designed to improve the efficiency and success of such referrals – through its live inventory function, care providers know that when they refer a client to seek resources at external agencies, the resources will be there. This function is interoperable with the shared care plans and allows providers to follow-up if clients are unable to obtain help through the referral.
-
Through its live inventory function, the Community Resource eXchange solves the issue of patients going somewhere only to find that the resource is no longer available. Patients will receive the right resources at the right time to appropriately address social and clinical barriers to health.
-
Over time, as we track which resources are in highest demand, we will be able to shine light on community-specific needs.
Community Care Coordination - Facilitates cross-agency care coordination
Our Community Care Coordination is a scalable model to provide compassionate care coordination across medical and social domains for Houston’s most vulnerable patients.
Care coordinators and case managers at partner agencies bring the model to life by using our comprehensive, shared, web-based health record system.
Our comprehensive health record system stores records of all patient visits to participating agencies, telling a complete story of where a patient has been and why. Access to the record is dependent on a viewer‘s role and HIPAA designation. Our Community Care Coordination model facilitates patient-centered care by structuring care plans around patients’ values and goals.
The software has been designed to continually record and analyze key data points around social determinants of health, which will ultimately inform policy on a local, state and federal level.
-
Not only will providers be able to see at which other agencies their patients receive services, but they will be able to read patient’s goals and values before meeting with patients. When providers know what is important to their clients, they can use goal-negotiated care models to achieve greater patient compliance and buy-in, and ultimately better health outcomes.
Our pilot program, in which our in-house care coordinators used our comprehensive health record system to document and measure patient outcomes, demonstrated measurable impact: It resulted in 54% reduction in hospital visits, 16% improvement in patient quality of life measures (DLA-20), and $5 Million in cost avoidance. This model, when scaled, promises to significantly improve the health safety net for Harris County’s most vulnerable patients, while saving the system millions of dollars.
To magnify the impact of this program in the community, our plan is to scale internal care coordinators to serve 150 clients/year, plus facilitate care coordination for an additional 1,500 clients through community partnerships in the next three to five years.
-
Our comprehensive case management software has been designed with both social service and medical agencies in mind to deliver the best care possible to clients with complex social, medical and behavioral health needs. The software enables case managers from different agencies to collaborate and see how clients have progressed in behavioral and health goals.
-
The Community Care Coordination model shifts patient care from a model centered around solving problems to a model centered first and foremost around patient values to increase engagement and patient satisfaction across the continuum of care. Additionally, through interagency case management, patients have an advocate to help them navigate a confusing, overly complicated health system.
-
As we gather further evidence about which social and economic barriers to health affect our community the most, we will have grounds to advocate for policies and legal systems that support more equitable access to health and wellbeing.
21
partner organizations
1088068
client records
1521869
health records
8011386
social records
Who Benefits
Our innovation is driven by the belief that all people, regardless of social or economic stability, deserves quality and effective healthcare.
Patients and communities are the ultimate benefactors of our Platform; in serving them we’ve quantified impact and savings for:
Case Studies
Unified Care Continuum Platform breaks down silos in care for clients of Recovery and Rehabilitation Center
Problem
The Houston Recovery Center partnered with PCIC to address a lack of data sharing in the community. The Center noticed a very silo-based model of case management in the Houston area: Although they knew that their clients were interacting with a broad array of social and medical service agencies across the city, none of the agencies could see what care their clients were receiving outside of their own walls. This resulted in inefficient case management, and many missed opportunities to communicate and collaborate across agencies.
Solution
PCIC linked HRC’s patient visit data with over 8 million patient visit records that exist in our Community Data eXchange (through existing partnerships with other social and medical agencies). To make this data meaningful to HRC, we built a customized, de-identified (HIPAA protected) dashboard for HRC that shows which other provider systems their patients frequent, how often they frequent them, and what services they receive there. This aggregated all the providers and services that their patients were utilizing into a single, global perspective.

We serve complex, high cost clients. PCIC confirmed it. Now we clearly see the community providers that also serve our clients. The usage patterns and costs are staggering.
PCIC provides a platform to develop systems of care coordination to improve health outcomes. This opens a brand-new door to preserve community resources and manage population health.
Program Manager - Houston Recovery Center
Copyright ©
Healthcare for Special Populations. All rights reserved.
Team Site