What we do
PCIC is a nonprofit organization that leverages technology, health data sharing, and public health best practices to empower patients and providers to achieve enduring health outcomes and financial sustainability.
We work with local governments, hospital systems, health plans, federally qualified health centers (FQHCs), health maintenance organizations (HMOs) and social service agencies to streamline care coordination and patient data sharing.
How we operate
Population Health Research
- Evaluating client outcomes Read More
- Informing feedback loop between technology and intervention
We facilitate inter-agency data sharing
We’ve created a county-wide health database that links patient information from a variety of healthcare, law-enforcement and social services in Houston.
This enables us to track not only our current patients as they move between social and medical agencies, but also to actively identify and reach out to Houston’s most frequent and complex users of emergency services.
By linking records from the county’s ecosystem of providers, we identify service gaps in the community and pinpoint which services are overutilized.
Health record software built around patient values and goals
PCIC is iteratively developing a newer, better electronic health record software that that guides providers to see health from the patient's perspective.
Our software not only documents patient medical histories, but it also prompts providers to learn about patients' lifestyle goals and potential barriers to managing their own care.
Our data-driven technology identifies patients most likely to benefit from care coordination
If an individual goes to one of our partner emergency rooms ten times in a year, and/or is admitted to one of our partner hospitals four times in a year, our care coordination team is notified and we personally reach out to the patient.
Together, care coordinators and patients decide whether the patient's participation in our health intervention program would align with his or her lifestyle goals.
Interventions built on respect and trust
Our two-to-six-month health interventions aim to empower patients to develop sustainable strategies to manage their chronic conditions.
Our case managers connect clients to community resources, bolster their health literacy, and make sure that transportation, scheduling, and billing don't get in the way of quality care.
Learn more about patient stories here.
We closely monitor patient health outcomes
Our population health team, ensures that the intervention team has the tools they need to accurately track patient progress throughout the health intervention.
We track quantitative and qualitative data to constantly measure, inform and improve our services.
Learn more about our research and measured impact here.
Often called High-Cost, High-Need, the complex patient population describes those who have frequent contact with the medical system without measurable improvements in their health.
Complex patients often utilize a variety of social service agencies and healthcare facilities, yet different agencies have no way of tracking where a patient has been or which diagnoses/medications the patient has received. The lack of a comprehensive patient record is problematic for patients and providers alike: in many cases, patients receive redundant services, and providers have no way of tracking long-term patient outcomes.
- Of $3 trillion spent on healthcare in the US each year, 22% is used on poorly coordinated care for the top 1% of High-Need, High-Cost patients.
- In Harris County, there are 6,000 High-Need, High-Cost patients whose cost of care has exceeded $800M for Medicaid alone.
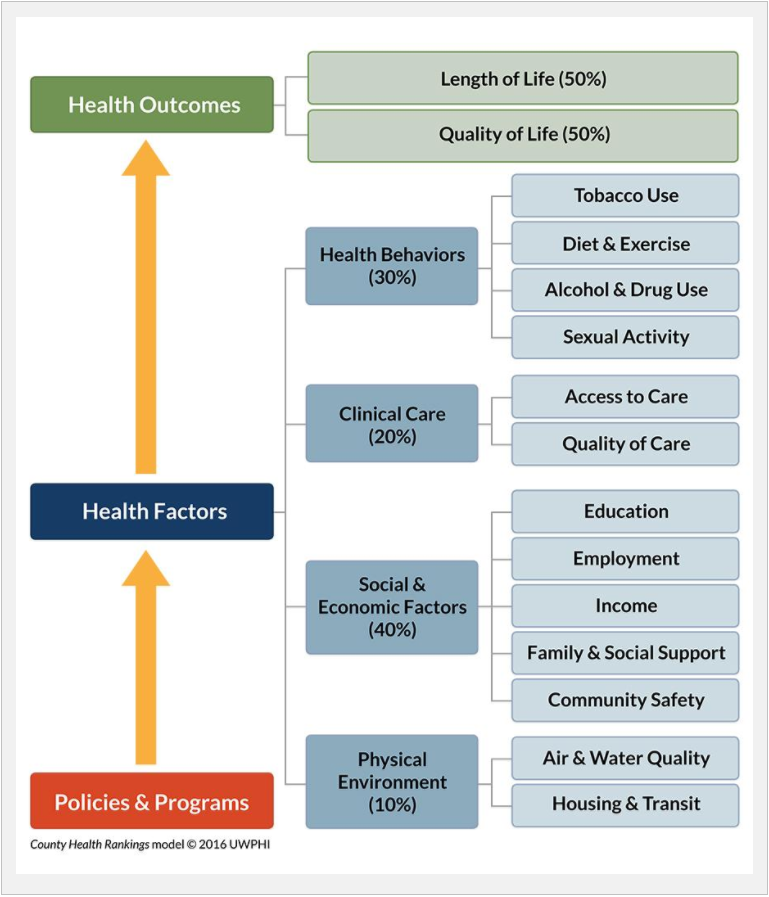
Our Unified Care Continuum Platform empowers providers to address social determinants of health
PCIC's healthcare technology product, the Unified Care Continuum Platform (UCCP) offers powerful community insights:
- Aggregate social and clinical data provides a big-picture view of where the most complex patients receive medical and social services, capturing the entire provider ecosystem all on one dashboard.
- Human-centered patient health records allow providers across agencies to document services and treatments offered to a patient. This electronic health record is unique for several reasons.
- It is designed around what is most important to a patient. For example, one patient may want to spend time with her mother and grandchildren above anything else, so a provider may frame medical treatment in the context of that goal.
- This health record identifies social and environmental risk factors for complex patients, thus empowering providers to identify risk factors specific to each patient and adjust care plans accordingly.
Often called High-Cost, High-Need, the complex patient population describes those who have frequent contact with the medical system without measurable improvements in their health.
Complex patients often utilize a variety of social service agencies and healthcare facilities, yet different agencies have no way of tracking where a patient has been or which diagnoses/medications the patient has received. The lack of a comprehensive patient record is problematic for patients and providers alike: in many cases, patients receive redundant services, and providers have no way of tracking long-term patient outcomes.
- Of $3 trillion spent on healthcare in the US each year, 22% is used on poorly coordinated care for the top 1% of High-Need, High-Cost patients.
- In Harris County, there are 6,000 High-Need, High-Cost patients whose cost of care has exceeded $800M for Medicaid alone.
Why PCIC is best-suited to help you effect lasting change
We are experts in primary care, health policy, public health research, data analysis, software development, social work, nonprofit management and more. Learn more about our team.
Fueled by curiosity and a drive to innovate, we are constantly improving our processes and outputs. Learn more about culture.