At PCIC we understand that health encompasses more than just physical symptoms of illness.
Health, as we define it, encompasses the complex interplay between medical, behavioral, and social factors.
Social Determinants of Health and Vulnerable Populations
What are Social Determinants of Health?
Social determinants of health refer to characteristics of the social environment that contribute to an individual’s health. These characteristics include economic, political, and legal structures, as well as social norms that determine how a society is organized and, by extension, the degree to which communities can access the resources necessary for health. For example, income, race, and zip code are all social determinants of health that are closely related to an individual and community’s likelihood of experiencing wellbeing.
How does evidence around Social Determinants of Health inform our model?
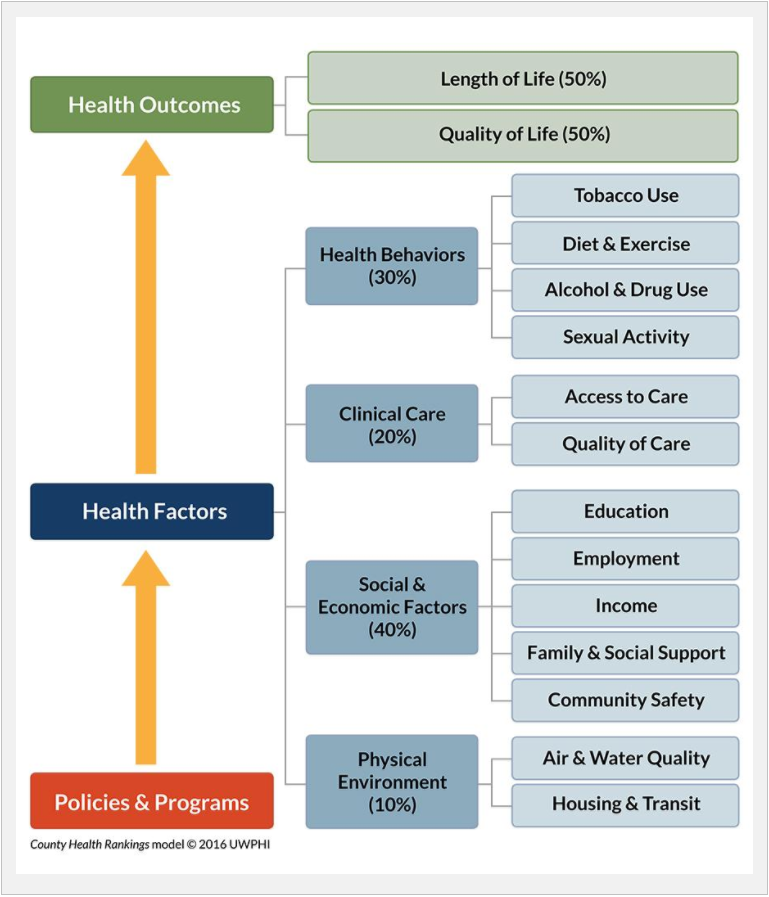
Evidence indicates that clinical care accounts for only 20% of health outcomes, while socioeconomic, behavioral, and environmental factors determine the remaining 80% (see Figure 1).
Given that social determinants of health often present an array of barriers that vulnerable patients must overcome in obtaining health and healthcare, we focus our work on developing intuitive technology through shared care plans that take these barriers into account.
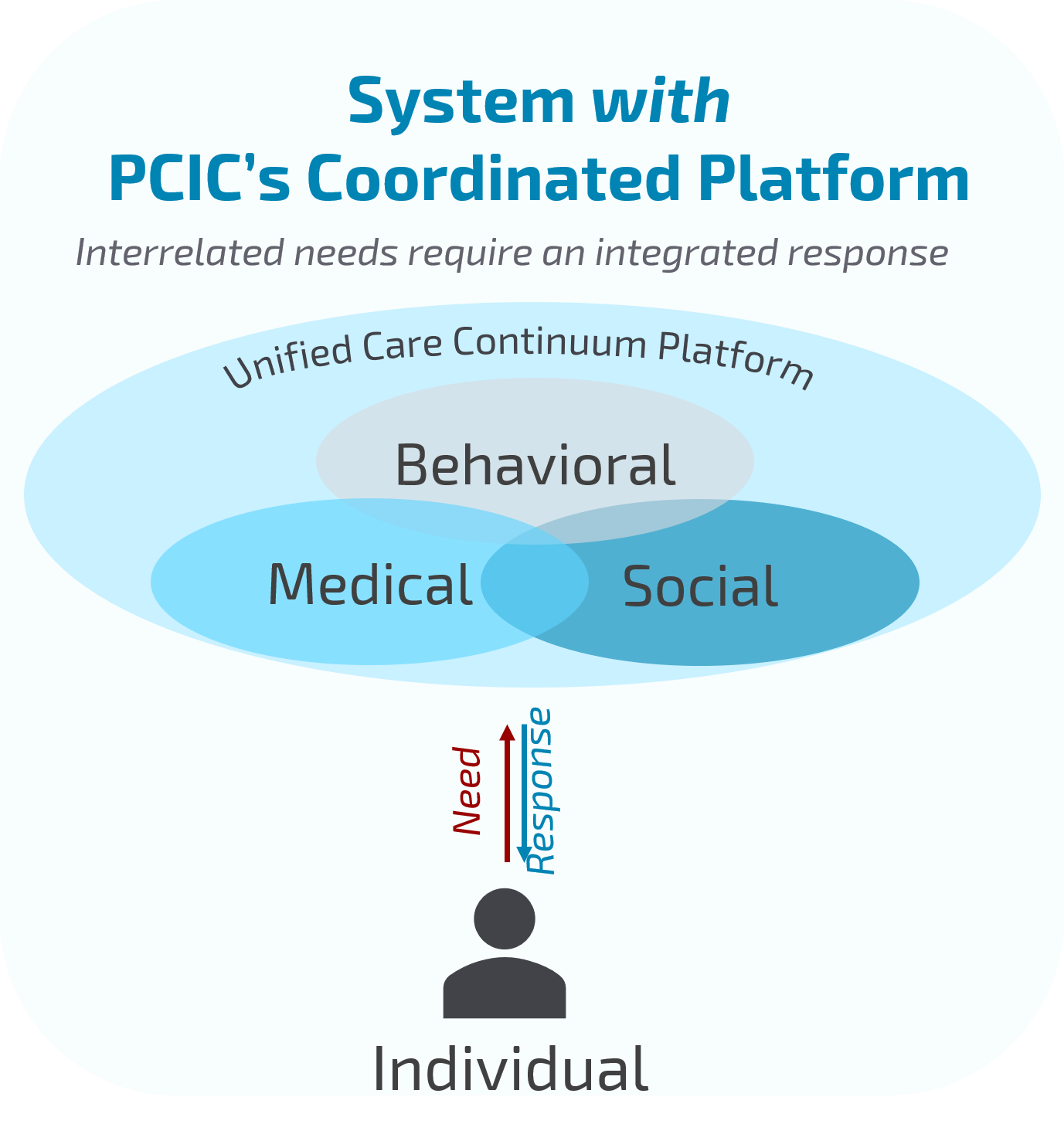
Our Unified Care Continuum Platform collects social determinant data to create feedback loops that will inform and improve systems of care.
How PCIC is moving the needle on Social Determinants of Health
PCIC envisions a system of care in which medical, behavioral, and social services are as interconnected as medical, behavioral, and social factors are in an individual’s wellbeing. Ultimately, the interplay between each of the domains of health requires an integrated system of care for vulnerable populations.
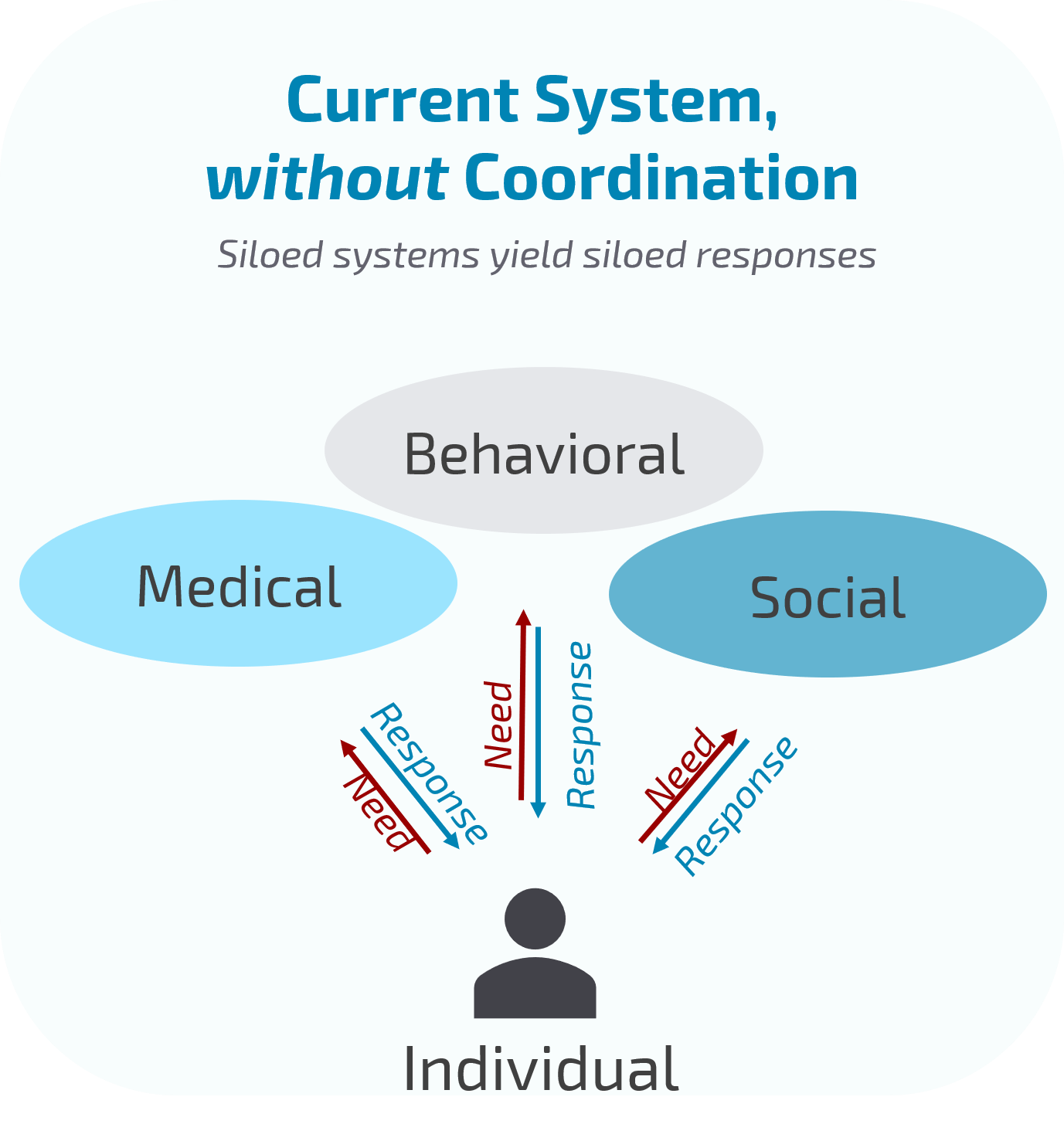
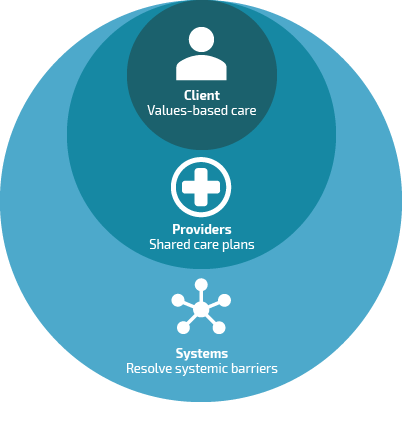
An integrated system of care must work on multiple levels to address the adverse impact of social determinants of health. We work to effect change and innovation on multiple levels through care coordination for patients with complex needs, collaboration with providers and their organizations, and advocacy for systems-level change.
Care Coordination for Patients with Complex Needs
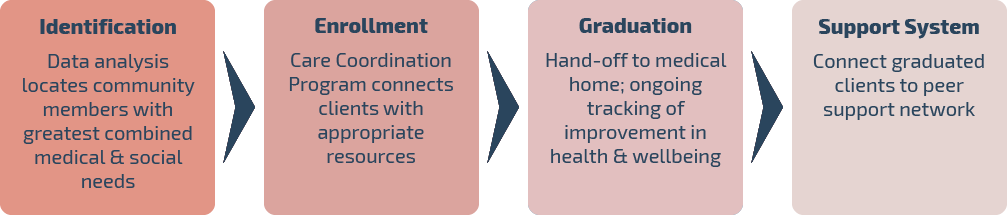
We support patients with complex needs in improving their quality of life and health outcomes by facilitating their access to resources and empowering patients to advocate for their needs and values with their providers.
PCIC’s Care Coordination team works directly with clients who utilize many social and medical services to meet needs that are unmet by the current healthcare system alone.
Our Care Coordination team is uniquely positioned to take a big-picture view of clients’ social and medical histories and needs, and connect them with resources that will have the greatest impact on their wellbeing – including, but not limited to, housing, behavioral health supports, health education services, and primary care homes.
By facilitating these referrals, our service helps clients overcome barriers to health caused by unfavorable socioeconomic, behavioral, or environmental factors. In doing so, our clients receive individualized support in navigating complex systems and experience improved quality of life and reduced utilization of healthcare services.
Collaborative Data Analytics with Providers and Organizations
We collect and assist organizations in analyzing data on medical, behavioral, and social service utilization.
Our data discovery and overlap analysis helps individual organizations see the full landscape of need and services their clients utilize across the entire community.
Our data analytics and shared client record widens the lens of agencies, enabling them to see each other’s work with clients and to more effectively collaborate in providing services.
In doing so, our work allows a constellation of agencies to respond collectively to the complex needs of those rendered most vulnerable by social and environmental determinants of health.
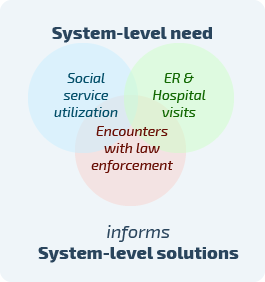
Advocacy for Systems-Level Change
Long-term solutions to our complex healthcare problems and improvements in population health will ultimately need to be driven at the policy level.
Our long-range impact strategy includes gathering widespread data to inform policymakers of our community’s most pressing and unmet needs.
By partnering to share data with agencies across medical, behavioral, and social service providers, we are drawing insights from a complex, data-rich landscape. Our Unified Care Continuum Platform is designed to make sense of this data by identifying barriers in accessing care as well as gaps in services received. Additionally, our platform tracks social and medical service utilization, a proxy for unmet need and disparity.

Gathering and analyzing this data is the first step in understanding the unique strengths and needs of our community’s health system. By turning insights into systems-level feedback loops, we are working to play a key role in helping policymakers develop evidence-based decisions to reduce health disparities and improve population health.
Definitions
How do we define Health?
The state of complete physical, mental, and social wellbeing and not merely the absence of disease or infirmity.
At PCIC we understand health encompasses more than just physical symptoms of illness. Health, as we define it, encompasses the complex interplay between medical, behavioral, and social factors.
We also believe that the potential for individuals and communities to heal and thrive requires the presence of interconnected, humanizing sources of support. Resilience through illness and health are created within AND beyond the healthcare system. Wellbeing requires the presence of individual-, provider-, and community-level supports.
How do we define Healthcare?
Our understanding of health requires us to expand our definition of healthcare to include an array of services and interactions that foster wellbeing across medical, behavioral, and socioeconomic domains.
At PCIC, healthcare occurs on multiple levels and in a variety of settings between individuals and their medical, behavioral health, and social service providers.
We believe that the quality of care individuals and patient populations receive is a direct result of the degree to which providers and systems work together to support the multiple aspects of an individual’s wellbeing.